skip to main |
skip to sidebar

This looks at the relapse risk over 5 years. These are remitted patients who go off medicines, and we're following them over time to see if their symptoms come back. Relapse was defined as rehospitalization, a very stringent criteria for relapse. And by 5 years, almost all patients had relapsed.
If you look at the group of patients who had had a first relapse and were followed out over time, 60 were at risk. Almost all had a second relapse, and then a third relapse was inevitable, happening more quickly. So relapse risk is very high, not necessarily in the first weeks after medication discontinuation or even in the first months, but over this time period symptoms will come back.
Enhancing Outcomes by Addressing Critical Challenges in the Treatment of Schizophrenia

A larger number of previous episodes of affective disorder was associated with poor antimanic response to lithium but not to divalproex. This differential treatment response did not result from current rapid cycling or mixed states.
Explanations for reduced response to lithium in subjects with many previous episodes include the following: 1) Lithium resistance may develop with repeated episodes (2). Reduced response to lithium prophylaxis has been reported in patients with many episodes and early onset (3) and in those with more than three previous manic episodes (11). 2) Multiple lithium discontinuations could result in refractoriness to lithium. Most patients, however, have similar responses before and after lithium is discontinued (12, 13). Furthermore, in this study, previous response to lithium predicted current response (4). 3) A group of patients may have frequent episodes that were always lithium resistant, representing an inherently unstable subtype of bipolar disorder. If this proves true, early identification of such patients will be valuable in establishing lifetime treatment strategies.
These results are related only to treatment of acute mania. Further studies are needed to determine whether these relationships extend to maintenance treatment.
Differential Effect of Number of Previous Episodes of Affective Disorder on Response to Lithium or Divalproex in Acute Mania
OBJECTIVE: To review the pharmacology, pharmacokinetics, efficacy, and safety of milnacipran and evaluate relevant clinical trial data.
DATA SOURCES: MEDLINE, International Pharmaceutical Abstracts, and Google Scholar searches (1966–June 2010) were conducted using the key words fibromyalgia, milnacipran, and serotonin-norepinephrine reuptake inhibitor. Searches were limited to articles published in English.
STUDY SELECTION AND DATA EXTRACTION: All available English-language articles of human studies were evaluated. One pharmacokinetic study reviewed included animal data. References cited in identified articles were used for additional evaluation.
DATA SYNTHESIS: Milnacipran is a serotonin-norepinephrine reuptake inhibitor with a 3-fold increased selectivity for norepinephrine compared to serotonin. It is well absorbed with 85–90% bioavailability. Maximum concentrations are achieved 2–4 hours after administration. Milnacipran does not undergo cytochrome P450 metabolism and has a half-life of 6–8 hours. Fifty-five percent of each dose is excreted unchanged in the urine. Dose adjustment is needed in patients with an estimated creatinine clearance of <30 mL/min. Clinical trials indicated that twice-daily dosing at 100 mg/day or 200 mg/day was superior to single-daily dosing. Studies further established the effectiveness of both doses in the treatment of fibromyalgia pain utilizing patient self-reported pain scores, as well as on a visual analog scale, Patient Global Impression of Change scale, and the Short-Form 36 Physical Component Summary. A 6-month extension trial, which evaluated patients continued on milnacipran for up to 1 year, demonstrated continued pain relief. The most common adverse drug reaction associated with milnacipran was nausea, which was reduced with slow-dose titration and administration with food.
CONCLUSIONS: Milnacipran is an effective treatment option for patients with fibromyalgia. More head-to-head clinical trials are necessary to assess its ultimate place in therapy.
Milnacipran for Treatment of Fibromyalgia
There are many possible explanations for this lack of concordance, Dr. Alter said. "Probably the most prominent is the fact that chronic fatigue syndrome is a symptom complex, and there is no specific tissue you can biopsy or no specific test in CSF patients. It's probably a spectrum of patients, and some may be associated with XMRV or MLV and others due to other agents or no viruses at all. That has to be sorted out."
More Evidence Links Murine Virus to Chronic Fatigue Syndrome
"This study elegantly demonstrates how memantine is able to protect neurons without causing harmful side effects," said Giles E. Hardingham, BSc, PhD, professor of molecular neurobiology, University of Edinburgh in the United Kingdom, who was not involved in the study.
"Memantine only blocks NMDA receptors when they are engaged in harmful activities away from the synapse; it does not interfere with the normal functioning of the NMDA receptor at the synapse," Dr. Hardingham explained.
Memantine's Unique Mechanism of Action Uncovered

The sensitivity analysis demonstrated only a small potential confounding effect on the association between asthma and suicide. But Ferri said it is possible that depression may play a mediating role in suicide—individuals who developed depression after baseline might, for instance, have been more likely to interpret respiratory symptoms as a serious medical disorder, especially when symptoms were persistent and severe. (The sensitivity analysis is posted online at AJP in Advance as a data supplement to the article.)
Asthma, Air Pollution Linked to Increased Suicide Risk
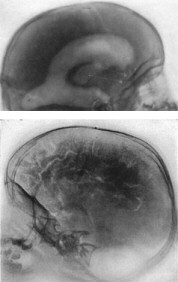
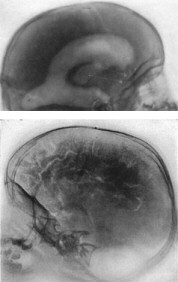
The crucial difference that struck Walter Dandy was the possibility of distinguishing flesh and air on an x-ray.
Knowing that the brain is surrounded by cerebrospinal fluid (CSF), which also fills internal spaces called the ventricles, he decided to simply replace the fluid with air and x-ray the patient.
He published his first results in 1918. He described how he drilled a hole in the skull of a patient and carefully removed the CSF from the ventricles and replaced it with air.
The following year he published another study where he deliberately filled this space with air as well, so the surface of the brain was surrounded by the gas and so could show up on an x-ray.
Neuroimaging, before the invention of television
Medscape: What is the risk for epilepsy in autism?
Dr. Chez: The risk for epilepsy in autism is 10%-30%, and it usually develops in the teenage or early adult years. Children with autism who are lower functioning, with mental retardation and cerebral palsy, for example, are more likely to develop epilepsy.
In addition, there are many children with autism who demonstrate epileptic spikes when monitored on 24-hour electroencephalography, but who do not manifest clinical epileptic seizures. These may be worth treating with antiepileptic drugs, as treatment may lead to improved behavior and receptive language. If the spikes are in the central temporal region, affecting the language area, I will usually try a trial of valproic acid. Valproic acid may also act as a mood stabilizer in these children, and also inhibits interleukin 1 cytokines, which may provide additional benefit. Other antiepileptic drugs may also be effective, although I have not seen good results with carbamazepine. There is also anecdotal evidence of improvement with the ketogenic diet.
Dr. Pellock: This is a controversial area. There are a few cases where treatment of epileptic spikes has resulted in improved behavior. However, without a clear manifestation of seizures, it is frequently difficult to know whether the short and long-term risks of the medications are really warranted. Clear goals need to be established to determine whether the treatment benefits the child. As a routine, I do not treat isolated spikes on the electroencephalogram, just as I would not treat isolated spikes in any child, with or without autism.
An Update on Autism -- Perspectives and Treatment: Autism and Epilepsy

#
Although there is strong evidence that light therapy can counter seasonal depression, the efficacy of light therapy as a treatment for major depression is less well established. Also, it looks as if light therapy might be more effective against major depression if it is combined with an antidepressant than if used alone.
In one randomized, controlled trial, for instance, 102 subjects were treated with the SSRI sertraline (50 mg/d). Subjects also received randomized augmentation treatment with 30 minutes of either bright morning (10,000 lux) or dim red (50 lux) light for five weeks. All clinician and self-report measures significantly favored active light augmentation.
#
Regarding St. John's wort, trials suggest that it is more effective for mild to moderate depression than for the severe form of the illness.
#
Studies have failed to demonstrate the efficacy of acupuncture compared with a control condition for the treatment of major depression.
#
And as for folate, its efficacy as a monotherapy for major depressive disorder has yet to be adequately tested. A few trials have found folate to be efficacious and well tolerated, although the best dose and form of folate remain unclear.
Alternative Treatments May Have Some Use in Depression
Психозы (феномены) «гиперчувствительности»
Клинически психозы гиперчувствительности проявляются обострением либо утяжелением симптомов психоза при назначении или смене антипсихотика. Первые клинические описания относятся к началу 60–х годов прошлого века, когда в начале нейролептической терапии на этапе титрации дозы у некоторых больных, преимущественно с органически неполноценной почвой и пожилых, отмечалось резкое усиление психоза. При этом в последующем, при увеличении дозы состояние, как правило, достаточно быстро стабилизировалось. В основе данного феномена – артефактное усиление дофаминовой трансмиссии вследствие гиперчувствительности постсинаптических D2–рецепторов и увеличения их плотности. В последние годы данный клинический феномен регистрировался также при переводе с обычного антипсихотика (антагониста D2–рецепторов) на частичные агонисты дофамина. В данном случае механизм феномена гиперчувствительности несколько иной: высокий аффинитет к данному типу рецепторов и несколько иной профиль активности обусловливает вовлечение новых, ранее не задействованных рецепторов и частичное усиление синаптической трансмиссии в начале терапии.
Конечно, не каждое усиление психотических симптомов после перевода на новый препарат является феноменом гиперчувствительности. Четкая дифференциация с обострением психоза, безусловно, необходима. Одним из опорных признаков может быть тот факт, что риск обострения у стабильных больных низкий в первые 2–3 недели после отмены/перевода и повышается в последующие месяцы. Согласно данным многочисленных обсервационных исследований к факторам риска обострения следует отнести: мужской пол, молодой возраст, наличие органической почвы, зависимостей. Также выше риск обострения у стационарных и недавно стабилизированных пациентов, при резком обрыве терапии, предшествующей терапии высокими дозами АП и клозапином.
Терапевтическая тактика при психозах гиперчувствительности заключается в усилении антипсихотической терапии с быстрым повышением дозы. В то время как при переводе с D2–антагониста на частичный агонист тактика должна быть принципиально иной, с более медленной сменой антипсихотика.
«Ранняя активация» пациента при смене антипсихотика
«Ранняя активация» (РА) – достаточно часто используемое в последнее время определение в литературе. Следует отметить, наряду с «непривычностью» термина для психиатров, также отсутствие четкой клинической дефиниции. В целом под РА понимается развитие у пациента в начале новой антипсихотической терапии избытка энергии, повышенной активности, инсомнии. Традиционно данная симптоматитка рассматривалась как стимулирующий эффект нового препарата, что справедливо воспринимается, как нежелательное явление у психотических больных либо как признаки утяжеления психоза. Вместе с тем клинический феномен РА связан с отменой предшествующего антипсихотика и рассматривается исключительно как эффект отмены. Он связан с прекращением блокады гистаминовых рецепторов 1 типа (H1) и развивается при резкой отмене препаратов, фармакологический профиль которых характеризуется высокой активностью к данному типу рецепторов. К таким препаратам относятся большинство седативных (низкопотентных) антипсихотиков (хлорпромазин, левомепромазин и др.), а также оланзапин и клозапин. Безусловно, в каждом конкретном случае необходим дифференциальный диагноз РА с акатизией, возбуждением и собственно редукцией седативного эффекта.
Терапевтическая тактика заключается в более медленной смене терапии, назначении бензодиазепинов, в том числе в целях профилактики.
Оптимизация тактики смены антипсихотической терапии на модели кветиапина
The first major breakthrough in the treatment of bulimia came with the era of SSRI antidepressant medications. The initial motivation was a perceived link between bulimia and depression, which commonly exist as co-morbid disorders. Serotonin was clearly involved in some way in the mechanisms of active bulimia. In 1997, Prozac became the first drug ever licensed by the FDA for the treatment of bulimia nervosa. The drug’s formal approval was based on clinical studies showing median reductions in binging of as much as 67 per cent for Prozac, compared with 33 per cent for placebo. Vomiting was reduced by 56 per cent, compared to 5 per cent for female placebo users. (About 10 per cent of diagnosed bulimics are males.) While cure is too strong a word, the benefits were quite dramatic in some cases.
What about the roughly 50% of bulimics who do not respond to serotonin-boosting medications? Recent research covered by the science blog Neurotopia points the finger at a long nerve running through the cranium. The tenth cranial nerve, better known as the vagus nerve, branches through the neck, thorax and abdomen, and is involved in breathing, tasting, swallowing, and digestion. Most of the signal traffic carried by the vagus nerve is one way: from the body to the brain. Suspicion fell on the vagus nerve because of its direct involvement with one of bulimia’s most salient traits — the inability to feel normal levels of fullness, or satiety.
Bulimics must eat more at a sitting than non-bulimics in order to feel satisfied. There is evidence of vagus nerve involvement in meal satiation, portion size, and, notably, control of vomiting. Researchers have suggested that bulimics have a relatively insensitive vagus nerve, made even less sensitive by the debilitating cycle of overeating and vomiting. Hence, bulimia patients need greater vagus nerve stimulation in order to stop eating. Interestingly, studies have also shown that people suffering from bulimia have high pain thresholds, compared to non-bulimics.
This dysregulation of the vagus nerve responds to the drug ondansetron, according to recent research published in Physiology & Behavior by Patricia L. Faris and colleagues. The antiemetic effects of ondansetron, which reduce vagus nerve activity by acting on the 5-HT3 serotonin receptor, seem to decrease vomiting while increasing the number of normal meals eaten.
Finally, a third path toward treatment has been sparked by research on opioid receptors. Decreased endogenous opioid activity may also underpin bulimia. A small 2005 study by Johns Hopkins University School of Medicine analyzed the results of brain MRIs on eight bulimic women and eight controls. Bulimics showed decreased opioid receptor binding in the insula, another area of the brain implicated in MRI studies of addiction. The insula has been called the brain’s “gustatory cortex,” and it may be that the repeating cycle of binge and purge activates the opioid system. Opioid receptors are involved in the processing of the reward value of food. This suggests that a drug like naltrexone, which blocks opiate receptors, might also have a role to play in the treatment of bulimia.
Drugs for Bulimia
The actions of S-adenosyl methionine in the central nervous system have been reviewed previously (3, 7, 8). SAMe acts as a major methyl donor for the synthesis of brain amines and maintenance of phospholipid cell membranes. Low levels of SAMe have been reported in the cerebrospinal fluid (CSF) of severely depressed patients. Oral and parenteral administration of SAMe result in a rise in CSF SAMe concentrations, indicating the compound crosses the blood-brain barrier. An increase in SAMe levels has been positively correlated with improvement in depression. SAMe concentrations also appear to rise in patients who respond to other antidepressants such as desipramine. SAMe is produced in the one-carbon cycle involving folate, homocysteine, and vitamin B12 and abnormalities of each of these compounds has been associated with depression. In short, the hypothesis is that abnormalities in the one-carbon cycle may result in low concentrations of SAMe that in turn may limit the synthesis of brain neurotransmitters such as serotonin, norepinephrine, and dopamine. This may directly contribute to depressive symptoms or interfere with or limit the action of other antidepressants. Administration of SAMe may ameliorate these deficiencies or augment antidepressants and facilitate neurotransmission.
In this issue, Papakostas and colleagues (1) report the results of an adjunctive trial of S-adenosyl methionine (SAMe) in 73 patients with major depression who had failed a prior selective serotonin reuptake inhibitor trial at an adequate dose for at least 6 weeks. Patients were randomly assigned to SAMe, with a targeted dose of 800 mg twice a day, or placebo. Both were added to the ongoing antidepressant regimen and continued for 6 weeks. Response according to the primary outcome, the Hamilton Depression Rating Scale (HDRS), was more likely with SAMe (36.1%) than with placebo (17.6%), as was remission (HDRS score ≤ 7): 25.8% versus 11.7%, respectively. Differences were statistically significant and clinically meaningful.
S-Adenosyl Methionine (SAMe) Augmentation in Major Depressive Disorder
Studies of mice and rats infected by T. gondii have shown risky behavior changes, including an attraction to the smell of cat urine that makes them vulnerable to attacks. These findings may have parallels in behavioral changes in people, from schizophrenia to depression and reflex impairment.
Glenn McConkey, a researcher at the University of Leeds in England, reported last year that two genes in T. gondii's DNA contain instructions for the production of an enzyme that makes a brain chemical called dopamine.
"That's somewhat unusual, because other parasites don't have that [dopamine]," said Sarven Sabunciyan, Yolken's colleague at Hopkins. After all, microbes have no brains.
But in higher animals with nervous systems, dopamine is a neurotransmitter with important roles in regulating behavior. Some anti-psychotic drugs used to treat schizophrenia work by blocking dopamine action in the brain.
In May, Hopkins researcher David J. Schretien published a study suggesting that some brain changes and cognitive symptoms in schizophrenics may be caused or worsened by exposure to a herpes simplex virus. A 2005 Czech study found evidence of personality changes in humans infected by another herpes virus called cytomegalovirus. And numerous studies have suggested that flu infections during pregnancy may increase a child's risk of schizophrenia and autism.
Evidence that T. gondii infections may be a cause of schizophrenia, while not yet conclusive, is growing, Yolken said. A review of past studies, published last year by Yolken and Torrey, collected a variety of intriguing correlations. For example: People with schizophrenia have a higher prevalence of T. gondii antibodies in their blood. There are unusually low rates of schizophrenia and toxoplasmosis in countries where cats are rare, and unusually high rates in places where eating uncooked meat is customary. And some adults with toxoplasmosis show psychotic symptoms similar to schizophrenia.
Studies have linked a history of toxoplasmosis with increased rates of other mental changes, too, including bipolar disorders and depression. A 2002 study in the Czech Republic noted slowed reflexes in Toxoplasma-positive people and found links between the infection and increased rates of auto accidents.
Still, the links between schizophrenia and toxoplasmosis are not simple. For example, most people infected with T. gondii never become schizophrenic. And not all schizophrenics have been exposed to toxoplasma.
Yolken believes additional factors, such as an unlucky combination of genes, are probably needed to produce schizophrenia among Toxoplasma-infected people. The parasite's DNA may also be important, since some strains are known to cause more disease.
Studies have also suggested that the timing of the infection — early in life when the brain is developing — and the place in the brain where the cysts settle, may be important, he said.
Yolken said that while T. gondii cysts are invisible to the immune system, they are not totally passive. Inside the cysts, the microbes are alive, sensing their environment, periodically trying to break out, multiply and form more dopamine-making cysts. The flare-ups probably occur when the host's immune system is weakened by illness or stress.
Sabunciyan has reported promising results with a class of anti-malarial drugs, called artemisinins, which appear to be effective at killing T. gondii in tissue cultures. "The next step is to do that in animals," Yolken said.
Yolken, a cat owner who says he has tested positive for Toxoplasma antibodies, said the potential link between Toxoplasma infections and mental illness is no reason for cat owners to panic — they just need to keep some basic hygienic precautions in mind.
Researchers explore link between schizophrenia, cat parasite